A global analysis released on Monday forecasts that drug-resistant superbugs could claim nearly 40 million lives over the next 25 years, prompting researchers to call for urgent action to avert this dire outcome. Superbugs, which are strains of bacteria or pathogens that have developed resistance to antibiotics, are increasingly recognized as a significant threat to global health. This analysis is the first of its kind to track the global impact of superbugs over time and to project future outcomes.
According to the GRAM study published in The Lancet journal, more than a million people worldwide succumbed to superbugs, also known as antimicrobial resistance (AMR), each year between 1990 and 2021. Notably, deaths among children under five decreased by over 50% over the past three decades due to improved measures for preventing and controlling infections in infants. However, when children do contract superbugs, the infections are now much more difficult to treat. Conversely, deaths among those over 70 have surged by more than 80% over the same period, as an aging population becomes more susceptible to infection.
The study revealed that deaths from MRSA, a type of staph bacteria resistant to many antibiotics, doubled to 130,000 in 2021 compared to three decades prior. Researchers used modeling to predict that, based on current trends, direct deaths from AMR could increase by 67% to nearly two million annually by 2050. Additionally, AMR could contribute to an additional 8.2 million deaths per year, a rise of nearly 75%. Under this projection, AMR would directly cause 39 million deaths over the next 25 years and contribute to a total of 169 million deaths.
However, more optimistic scenarios are also possible. If global efforts are made to enhance care for severe infections and improve access to antimicrobial drugs, it could save the lives of 92 million people by 2050, according to the modeling. The study examined 22 pathogens, 84 combinations of drugs and pathogens, and 11 infectious syndromes such as meningitis, using data from 520 million individual records across 204 countries and territories.
Co-author Mohsen Naghavi of the US-based Institute of Health Metrics emphasized that AMR has been a significant global health threat for decades and that this threat is escalating. Jeremy Knox, head of infectious disease policy at the UK-based health charity the Wellcome Trust, warned that the rising rates of AMR would have widespread consequences. He noted that a growing AMR burden, as described in the GRAM report, would steadily undermine modern medicine, as antibiotics essential for safe and routine medical interventions could lose their effectiveness.
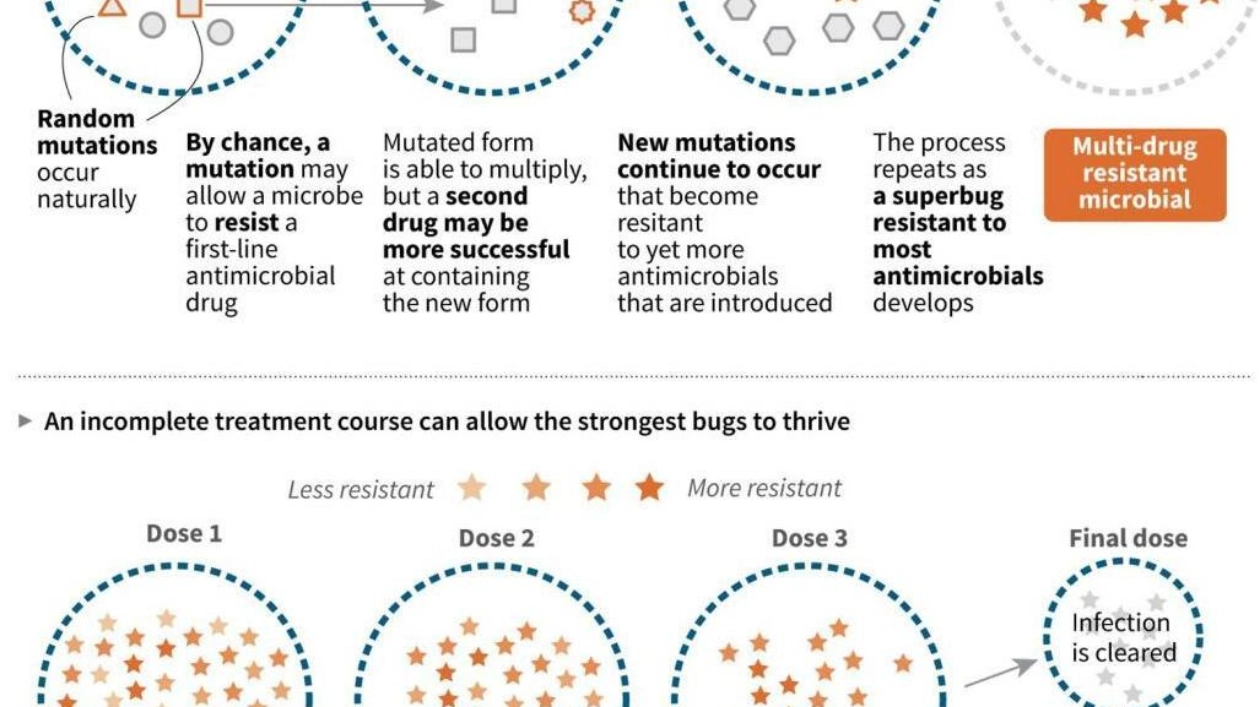
Although there has been a gradual increase in political attention to the issue over the past decade, Knox stated that governments worldwide have not yet taken sufficient or swift action to address the AMR threat. He highlighted the high-level AMR meeting at the United Nations scheduled for September 26 as a crucial moment in the fight against superbugs. Antimicrobial resistance is a natural phenomenon, but the overuse and misuse of antibiotics in humans, animals, and plants have exacerbated the problem.